Rotator Cuff Tear-related Degenerative Shoulder Arthritis
Reverse Total Shoulder Arthroplasty
(also known as Inverse Total Shoulder Arthroplasty)
— For those who have great difficulty lifting their shoulder —
If you have the following symptoms, the condition may be diagnosed as 'cuff tear arthropathy'.
【Symptoms】
1.Reduced range of motion in the shoulder, with a grinding or grating sound.
2.Little to no pain when the shoulder is at rest, but significant pain when moving it.
3.Difficulty lifting the arm above shoulder level (suggesting severe joint deformity). Inability to lift the arm to the side.
If you are experiencing these symptoms, it is possible that the bones in your shoulder have become deformed, as shown in the illustration.
In the diagram below, the left image shows a normal shoulder joint, while the right shows a deformed joint caused by cuff tear arthropathy.
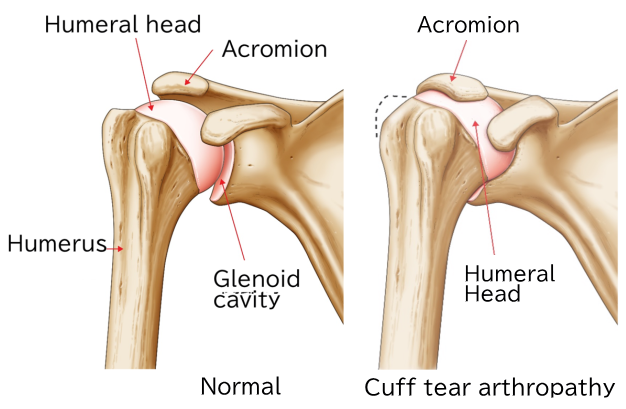
Difference from the Illustration
While not shown in the illustration, the key difference between a normal shoulder and one with cuff tear arthropathy is that the rotator cuff tendons (part of the inner shoulder muscles) covering the humeral head are severely torn. As a result, the humeral head comes into direct contact with the acromion.
【Treatment Policy】
【For patients whose main goal is pain relief and who do not need to move their shoulder much: 】
The first-line treatment is conservative therapy, as shoulder pain often improves with rest and corticosteroid injections into the joint to reduce inflammation.
【When the pain settles down】
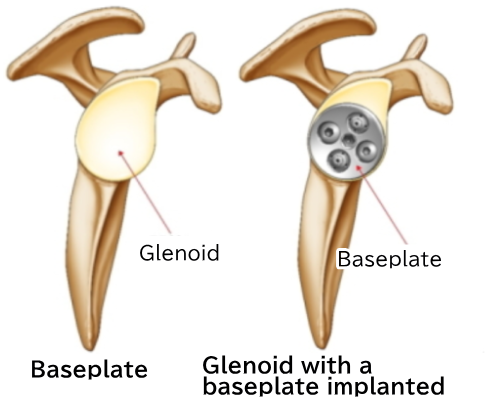
When shoulder pain begins to ease, exercise therapy is recommended. This is because, even with rotator cuff tear arthropathy, there are many cases where the arm can be raised. Why the arm can be raised even when the rotator cuff is torn is still not clearly understood. Also, in rotator cuff tear arthropathy, the glenoid (shoulder socket) of the scapula (please refer to the section on total shoulder arthroplasty) is often damaged. The degree of bone deformity varies from person to person. Therefore, some people benefit from exercise therapy, while others may not.
【If Conservative (Non-Surgical) Treatment Is Ineffective】
Several surgical treatment options are recommended.
1.Arthroscopic Synovectomy
This procedure involves using an arthroscope to examine the joint and clean out degenerated (non-healthy) tissue from the rotator cuff and synovium.
While this can reduce pain, improvement in shoulder mobility varies from person to person.
2.Hemiarthroplasty (Partial Shoulder Replacement)
This surgery replaces only the humeral head with an artificial component. Unlike total shoulder replacement, hemiarthroplasty does not involve the glenoid (socket side of the joint).
Improved range of motion can be expected in patients who were able to lift their arm despite experiencing pain prior to surgery.
However, in patients with significant pain and inability to lift the arm, hemiarthroplasty is less likely to improve shoulder function.
Therefore, the decision to perform hemiarthroplasty for cuff tear arthropathy is based on the patient’s symptoms and functional goals, and is carefully determined by the physician.
【A New Treatment Option for Patients Who Are Unable to Lift Their Shoulder】
There have been reports indicating the effectiveness of reverse total shoulder arthroplasty, which was approved for use in Japan in April 2014. This type of shoulder replacement has been in use since the 1990s in Europe and since 2004 in the United States.
Japan adopted this procedure much later compared to Western countries. As a result, clinical data originating from Japan and involving Japanese patients is still limited.
During my time studying abroad in the United States, I observed several cases of reverse total shoulder arthroplasty, including surgeries and postoperative outcomes. However, compared to physicians in the U.S. and Europe, I cannot say that I have extensive experience with this procedure.
The information provided below is based on the knowledge and observations I gained during my training overseas.
【Reverse Total Shoulder Arthroplasty】
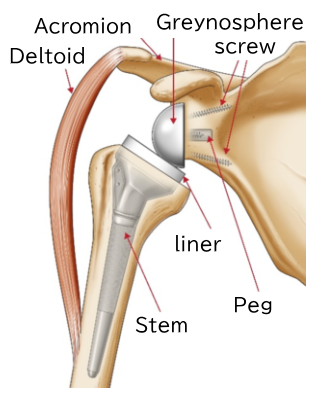
Reverse total shoulder arthroplasty involves implanting specialized components into the shoulder blade (scapula) and upper arm bone (humerus), as shown in the illustration below.
In this procedure, a plastic socket (liner) and stem are placed into the deformed humerus, while a metal ball (glenosphere) and baseplate are attached to the glenoid cavity of the scapula. The baseplate is secured using metal screws.
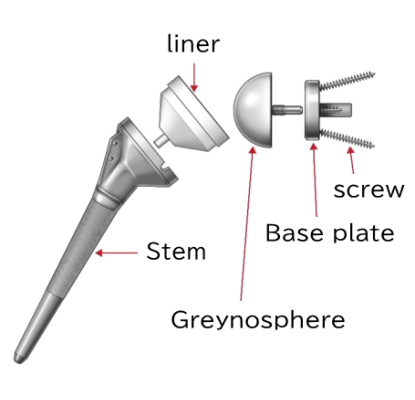
The diagram below shows the reverse shoulder prosthesis implanted into the humerus and scapula. The stem and liner are connected as a single unit.
The diagram below shows the baseplate implanted into the glenoid cavity of the scapula.
Why is it called a Reverse Total Shoulder Arthroplasty?
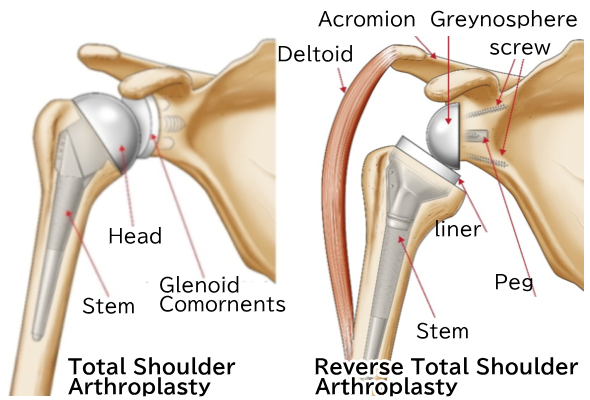
In total shoulder arthroplasty, the damaged humeral head is replaced with an artificial head, and the glenoid component is implanted into the damaged glenoid cavity. When the rotator cuff tendons (the tendons of the inner shoulder muscles) are intact, a standard total shoulder arthroplasty is usually performed (see the section on total shoulder arthroplasty). The structure of the shoulder after surgery closely resembles the original shoulder anatomy.
However, in reverse total shoulder arthroplasty, the ball component called the glenosphere is placed on the glenoid (socket) side, and the socket component is attached to the humeral side. In standard total shoulder arthroplasty, the ball is attached to the humerus, and the socket is implanted into the glenoid cavity. In the reverse procedure, the positions of the ball and socket are switched.
Therefore, it is called a "reverse" total shoulder arthroplasty.
【Preoperative and Postoperative X-rays of Reverse Total Shoulder Arthroplasty】
Normal X-ray
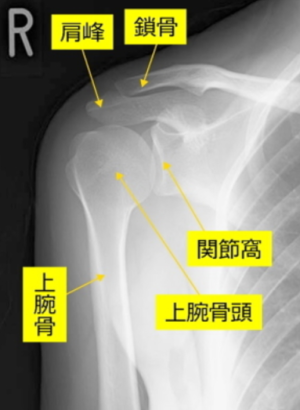
Preoperative X-ray (X-ray of cuff tear arthropathy)

Please refer to the illustration of cuff tear arthropathy. The space between the humeral head and the acromion is absent compared to normal.
Postoperative X-ray

The deformed humeral head has been removed, and implants (artificial components) have been placed in the scapula and humerus.
【Rehabilitation After Reverse Total Shoulder Arthroplasty】
Rehabilitation protocols vary between facilities, but generally, a brace is worn for several weeks. Gradual rehabilitation is then started. Based on my clinical experience in the United States, some patients are able to raise their arm to head level within about three months. However, the timing and extent of improvement in range of motion can vary greatly from person to person. Therefore, it is recommended to consult with your attending physician.
【Range of Shoulder Motion After Rehabilitation】
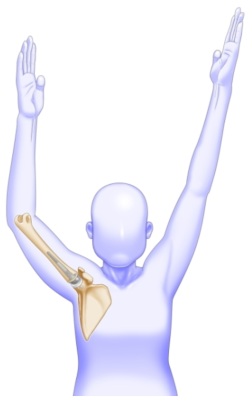
The illustration shows an average range of shoulder motion after rehabilitation. Please understand that it is difficult to achieve the exact same movement as the healthy side.
【Postoperative Course of Reverse Total Shoulder Arthroplasty (Case Example from an American Patient) 】
Here, we present a case example of a patient who underwent reverse total shoulder arthroplasty. These photos were kindly provided by Dr. Gerald Williams, where I studied abroad, with the patient's consent.
Dr. Williams is aware that this procedure was approved in Japan starting April 2014 and has expressed his support for the use of these photos to benefit future patients in Japan.
I would like to take this opportunity to express my sincere gratitude to Dr. Gerald Williams.
Postoperative progress at 3 months (right shoulder surgery)
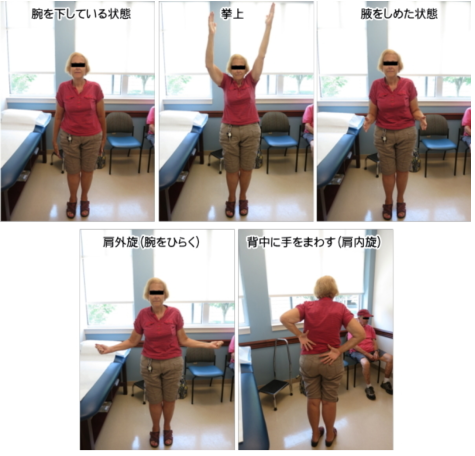
Postoperative progress at 2 years (left shoulder surgery)
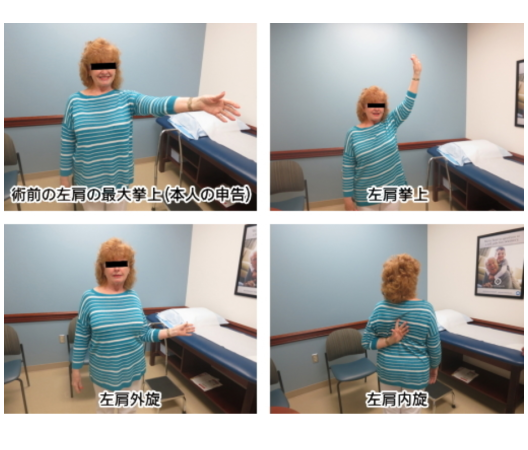
Postoperative progress at 5 years (right shoulder surgery)

【Recovery Milestones After Reverse Total Shoulder Arthroplasty】
1.Ability to Raise the Arm:
Some patients can raise their arm as early as three months after surgery, as shown in the photos. However, smaller women may have weaker deltoid muscles and might not regain full arm elevation as quickly.
2.External Rotation:
Generally, external rotation is limited. However, patients who had good external rotation before surgery often maintain relatively better external rotation afterward. Individual differences exist.
3.Internal Rotation (Reaching Behind the Back):
Regaining internal rotation after surgery is often difficult. Activities such as fastening a bra clasp or wiping oneself after using the toilet may be challenging. The degree of recovery varies between individuals.
4.Revision Surgery Cases:
Patients who have had previous surgeries may experience less improvement in range of motion after reverse total shoulder arthroplasty compared to those undergoing the procedure for the first time.
I will give you a rough idea of the typical course after surgery. In the past, the prognosis for joint replacement surgery was considered not very good. This was mainly because the plastic socket tended to loosen after a few years—that is, the plastic component would shift or come loose from the scapula, causing pain to recur.
However, thanks to recent advances in medicine, it is now expected that the implant may remain stable for about 10 years or more. These findings come from reports at leading centers where joint replacements are commonly performed worldwide, such as in the United States and France. Therefore, it is recommended to discuss with your attending physician how long your shoulder implant is likely to last.
Regarding activity levels—such as playing sports or how much weight you can safely lift—there is still no consensus. My mentor, Dr. Williams, advised patients not to lift more than 10 kg with both hands. Some of Dr. Williams’ patients have played golf after their shoulder replacement surgery. However, the extent to which patients can participate in sports depends on individual factors such as muscle strength, so there is variation from person to person.
Therefore, it is best to consult your physician about your activity level and how much weight you can safely lift after surgery.
【Specific Complications After Reverse Total Shoulder Arthroplasty】
Here, we will discuss representative complications that may occur during or after reverse total shoulder arthroplasty. Although complication rates have been reported by various medical centers worldwide, the numbers vary widely, so specific figures are not provided here. In Japan, clinical data are still insufficient, so please consult with your attending physician for more information.
1.Infection and Suppuration
An artificial joint is a foreign body to the human body. Infection can occur early after surgery or even later if the body's immune system weakens, allowing bacteria to invade around the implant and cause suppuration (pus formation). Signs of infection may include swelling of the shoulder, persistent fever, or sudden severe pain. During surgery, doctors take preventive measures against infection, such as administering antibiotics intravenously and thoroughly washing the area to minimize bacterial contamination. However, infection remains a possible postoperative complication. Infection rates vary between facilities, so specific numbers are omitted here. For reference, at Thomas Jefferson University, where I studied abroad, the infection rate after primary surgery was explained to patients as approximately 4%.
2.Nerve Injury
To correctly position the implant in reverse total shoulder arthroplasty, muscles may be retracted, and joint ligaments may be cut. During these maneuvers, transient nerve injury (such as numbness in the hand or difficulty bending the elbow for a few days) can occur due to traction on the arm.
3.Scapular Notching
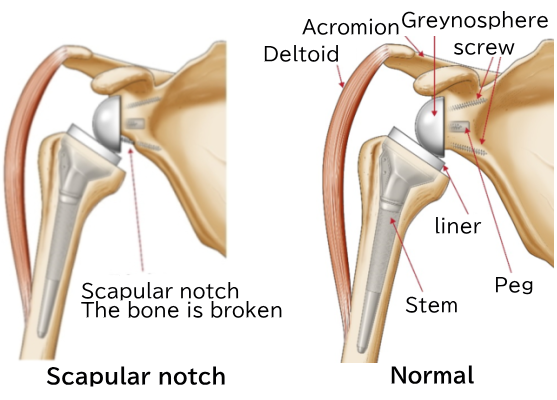
With the implant design of the reverse total shoulder arthroplasty, the motion of touching the opposite shoulder with the arm is more limited compared to a normal shoulder. When performing this motion (called shoulder adduction and internal rotation), the liner and the scapular bone can come into contact. Repeated contact causes wear of the scapula, which is known as scapular notching.
Symptoms may include noises during shoulder adduction and internal rotation. Severe pain is usually not reported. However, the liner gradually wears down, and X-rays show erosion of the scapular bone. Currently, there is no established treatment to repair the bone erosion caused by scapular notching.
Therefore, it is essential to take great care when placing the glenosphere to prevent scapular notching. Sometimes, adjustments such as changing the size of the glenosphere are made to address this issue. The frequency of scapular notching varies between medical centers.
For these reasons, it is recommended to thoroughly discuss with your attending physician how scapular notching is managed before undergoing surgery.
4. Acromion fracture
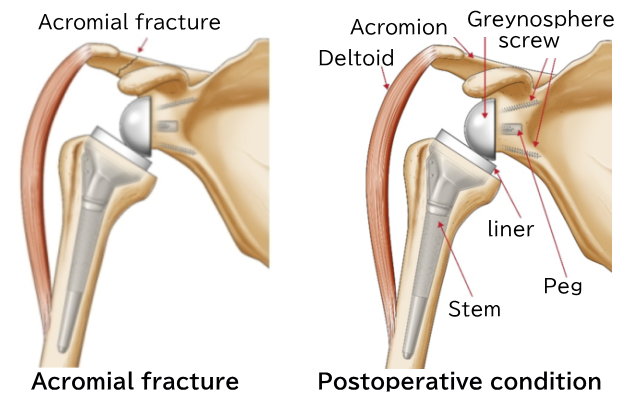
A fracture of the acromion may occur after surgery. The length of the upper limb may become somewhat longer. The humerus is supported by the deltoid muscle, but if the upper limb becomes too long, the deltoid is stretched, which can cause a fracture of the acromion where the deltoid attaches.
【Measures Against Complications After Reverse Total Shoulder Arthroplasty】
1.Against Infection
Depending on the severity, revision surgery may be necessary. For infections, antibiotics are administered intravenously, and the surgical site is cleaned. However, there are cases where the infection does not resolve. Depending on the extent of the infection, it may be necessary to completely remove the prosthesis at once. Revision surgery may also be required if the prosthesis becomes loose.
A common aspect of revision surgery involves the glenoid (the socket of the scapula), where the plastic liner is inserted and bone loss often occurs. Replacing the plastic liner again during revision surgery is very difficult. Therefore, even if the implant is ultimately replaced, it is often limited to reimplanting the metal ball and stem on the humeral side.
However, revision surgery is very challenging, so it is important to discuss it thoroughly with your attending physician.
2.Against Scapular Notching
As mentioned earlier, there is no established treatment to repair scapular notching once it occurs. Therefore, measures are taken to prevent scapular notching from happening in the first place. Specifically, careful attention is paid to the placement of the glenosphere, and its size may be adjusted. However, even with these measures, scapular notching cannot always be avoided.
3.Against Acromion Fracture
Unfortunately, if an acromion fracture occurs, conservative treatment such as immobilization with a brace is used to reduce shoulder pain. It is said that even if an acromion fracture happens, once the fracture heals, the range of motion of the shoulder will improve. However, there are individual differences, and in some cases, the range of motion may not improve sufficiently after the fracture. Therefore, if this occurs, please consult with your attending physician.
【Summary Regarding Rotator Cuff Tear Arthropathy】
1.Reverse total shoulder arthroplasty (reverse TSA) has been reported to be effective for rotator cuff tear arthropathy in cases where the shoulder cannot be raised at all.
2.In Japan, reverse total shoulder arthroplasty has been available since April 2014.
3.Since several possible complications may occur, please consult thoroughly with your attending physician before deciding on surgery.
Artificial Joints

In cases of degenerative shoulder arthritis where conservative treatments do not alleviate symptoms and the patient seeks pain relief and improved mobility, joint replacement surgery is recommended.
- What is Total Shoulder Arthroplasty?
- Anatomical Total Shoulder Arthroplasty (Total Shoulder Replacement Surgery)
- Rotator Cuff Tear-related Degenerative Shoulder Arthritis
- Joint Replacement Surgery for Patients with Rheumatoid Arthritis
- Revision Shoulder Arthroplasty (Replacement Surgery for Artificial Shoulder Joints)
- Postoperative Outcomes of Total Shoulder Arthroplasty in Elderly Patients
- Is Returning to Sports Possible After Reverse Shoulder Arthroplasty?
