Joint Replacement Surgery for Patients with Rheumatoid Arthritis
関節リウマチに対する人工肩関節置換術
~For those who have been told that surgery is difficult due to severe bone deformity~
Why is shoulder surgery difficult when the joint is severely deformed?
- For shoulder joint replacement surgery to be successful, the implant must be securely fixed to the bone and positioned correctly.
- When the shoulder is severely deformed, it is often difficult to place the implant properly.
Why Implant Placement Can Be Difficult
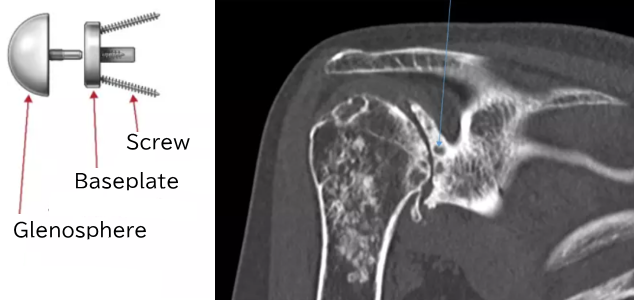
- In total shoulder arthroplasty, the implant placed in the glenoid (shoulder socket) is typically fixed with bone cement. However, over time, this implant may become loose. If the glenoid implant loosens, it can lead to increased shoulder pain.
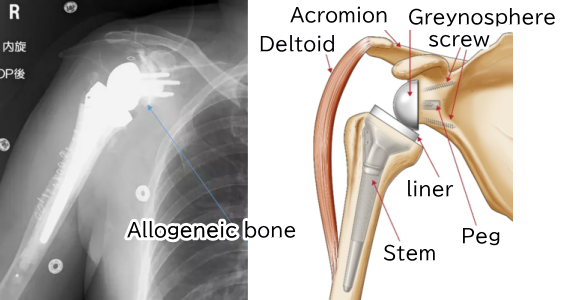
- In reverse shoulder arthroplasty as well, if the glenosphere (the implant placed in the glenoid) is not positioned optimally, there is a risk of loosening. This is because in cases of severe bone deformity, the amount of bone in the glenoid is often insufficient. As a result, the fixation of the glenosphere, which is secured to the glenoid with screws, may not be adequate.
What Type of Shoulder Prosthesis Is Suitable When There Is Severe Bone Deformity and Glenoid Bone Loss?
- When there is bone loss in the glenoid (shoulder socket), either allograft (donor bone) or autograft (the patient's own bone) is transplanted to the glenoid before placing a standard implant.
- The technique of grafting bone to the deficient glenoid and then performing reverse shoulder arthroplasty is called "bio-reverse.
Indications for the Bio-Reverse Technique
- Severely deformed shoulder joints that have not responded to conservative (non-surgical) treatment.
- In particular, patients with long-standing rheumatoid arthritis often have significant glenoid bone loss. Such patients are more likely to be good candidates for the bio-reverse technique.
A Case Example of a Patient with Rheumatoid Arthritis
- Female
- Age at the time of surgery: 70 years old
- Right shoulder pain
Range of motion before surgery

X-ray before surgery

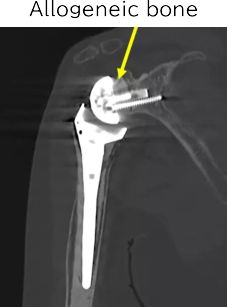
Coronal CT
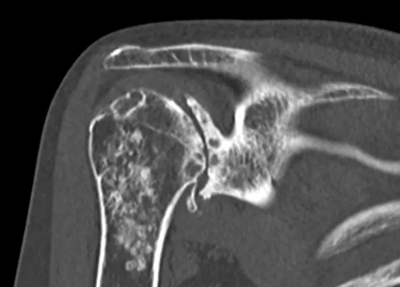
A deeply concave glenoid
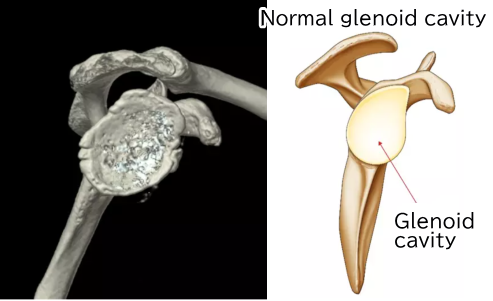
The glenoid at the time of surgery. It is shaped like a bowl.
Normally, the baseplate is fixed to the glenoid with screws.
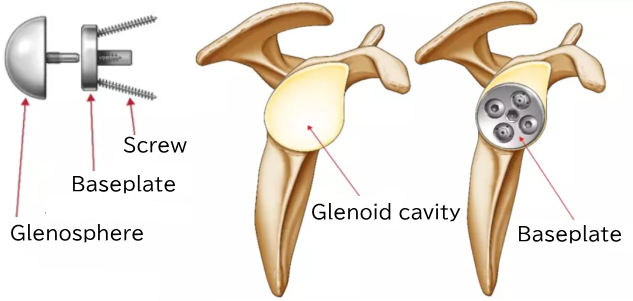
If the glenoid is deformed, the shape of the baseplate may not fit the glenoid properly.
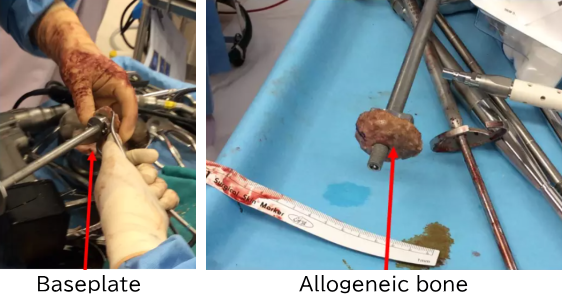
Therefore, a shaped allograft is attached to the baseplate to fit the deformed glenoid.
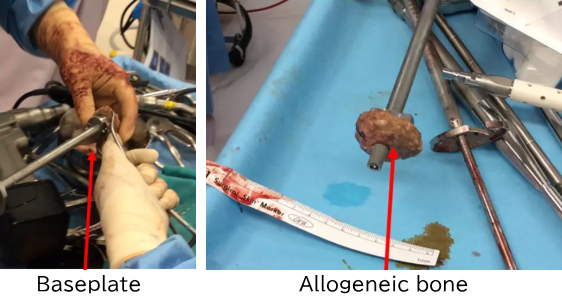
The baseplate with the allograft is fixed to the glenoid.
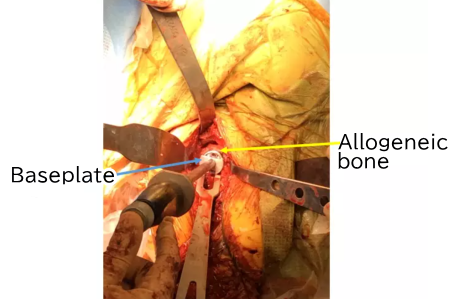
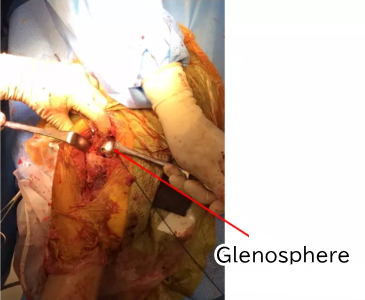
The glenosphere is attached.
Postoperative X-ray
Will the transplanted bone be maintained over time?
- We will show you the course over six years after surgery.
X-ray at six months after surgery

Shoulder range of motion six months after surgery

Shoulder range of motion one year after surgery

Shoulder range of motion two years after surgery
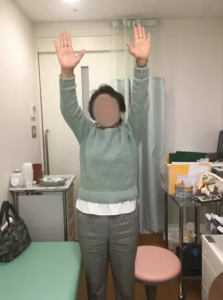
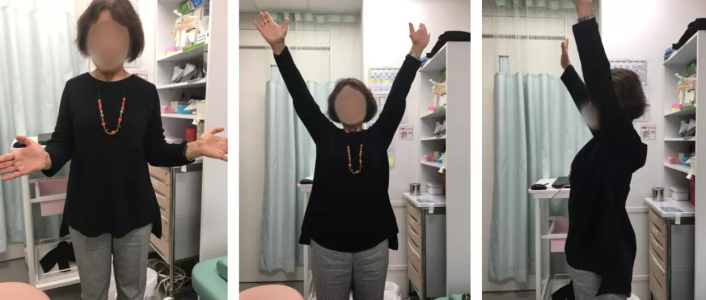
Shoulder range of motion six years after surgery
X-ray six years after surgery

CT scan six years after surgery
Current Condition of the Patient’s Right Shoulder
- There is no pain at all compared to before surgery.
- There is some stiffness in the shoulder.
- It is difficult to reach behind the back with the hand.
- There are no difficulties in daily life.
Seven Years After Surgery
This video shows the patient’s recent condition. Although she mentions difficulty reaching behind her back, she reports no problems with daily activities.
Summary
- In cases of severe shoulder deformity due to rheumatoid arthritis or similar conditions, the bio-reverse shoulder arthroplasty using allograft or autograft bone is an effective surgical option.
Artificial Joints

In cases of degenerative shoulder arthritis where conservative treatments do not alleviate symptoms and the patient seeks pain relief and improved mobility, joint replacement surgery is recommended.
- What is Total Shoulder Arthroplasty?
- Anatomical Total Shoulder Arthroplasty (Total Shoulder Replacement Surgery)
- Rotator Cuff Tear-related Degenerative Shoulder Arthritis
- Joint Replacement Surgery for Patients with Rheumatoid Arthritis
- Revision Shoulder Arthroplasty (Replacement Surgery for Artificial Shoulder Joints)
- Postoperative Outcomes of Total Shoulder Arthroplasty in Elderly Patients
- Is Returning to Sports Possible After Reverse Shoulder Arthroplasty?
